Hint's DPC Network
Hint Connect works in partnership with benefits innovators and employers to make Direct Primary Care (DPC) the standard of care for employer-sponsored health benefits through a curated network of DPC Clinicians.
Hint’s Direct Primary Care Network
Hint Connect works in partnership with benefits innovators and employers to make Direct Primary Care (DPC) the standard of care for employer-sponsored health benefits through a curated network of DPC Clinicians.
Benefit Advisors & Brokers
Tap into a nation-wide network of independent clinics to implement DPC for employers of all sizes.
Health Plans
Effortlessly integrate DPC into your overall plan design with a seamless member experience.
Employers
Improve employee satisfaction and care utilization, and save on healthcare costs.
Clinicians
Grow your practice through our relationships with larger, geographically diverse employers.
Add High Quality Primary Care to Your Employee Benefits Offering
Direct Primary Care (DPC) is a model that removes insurance from the doctor-patient relationship, enabling doctors to build more meaningful relationships with patients and patients to receive better quality primary care.
In the DPC model, employers pay a recurring membership fee to DPCs for the wellness, chronic disease management, and urgent care needs of their patients. Employees enjoy a stronger relationship with their primary care doctor and better access including virtual visits, same-day/next-day appointments and after hours availability.
Improve Health Outcomes
Reduce
Downstream Costs
Prevent and Manage Chronic Diseases

Value for Employers
DPC does not replace insurance but instead reduces the usage of insurance since 80% of healthcare needs can be accommodated via primary care.
With both reduced usage of traditional insurance and the added value of direct primary care, employers benefit from tremendous savings.
13%
Total claims cost reduction
22%
Reduction in outpatient charges
40%
Reduction in ER utilization rate/1000
20%
Reduction in hospital utilization rate/1000
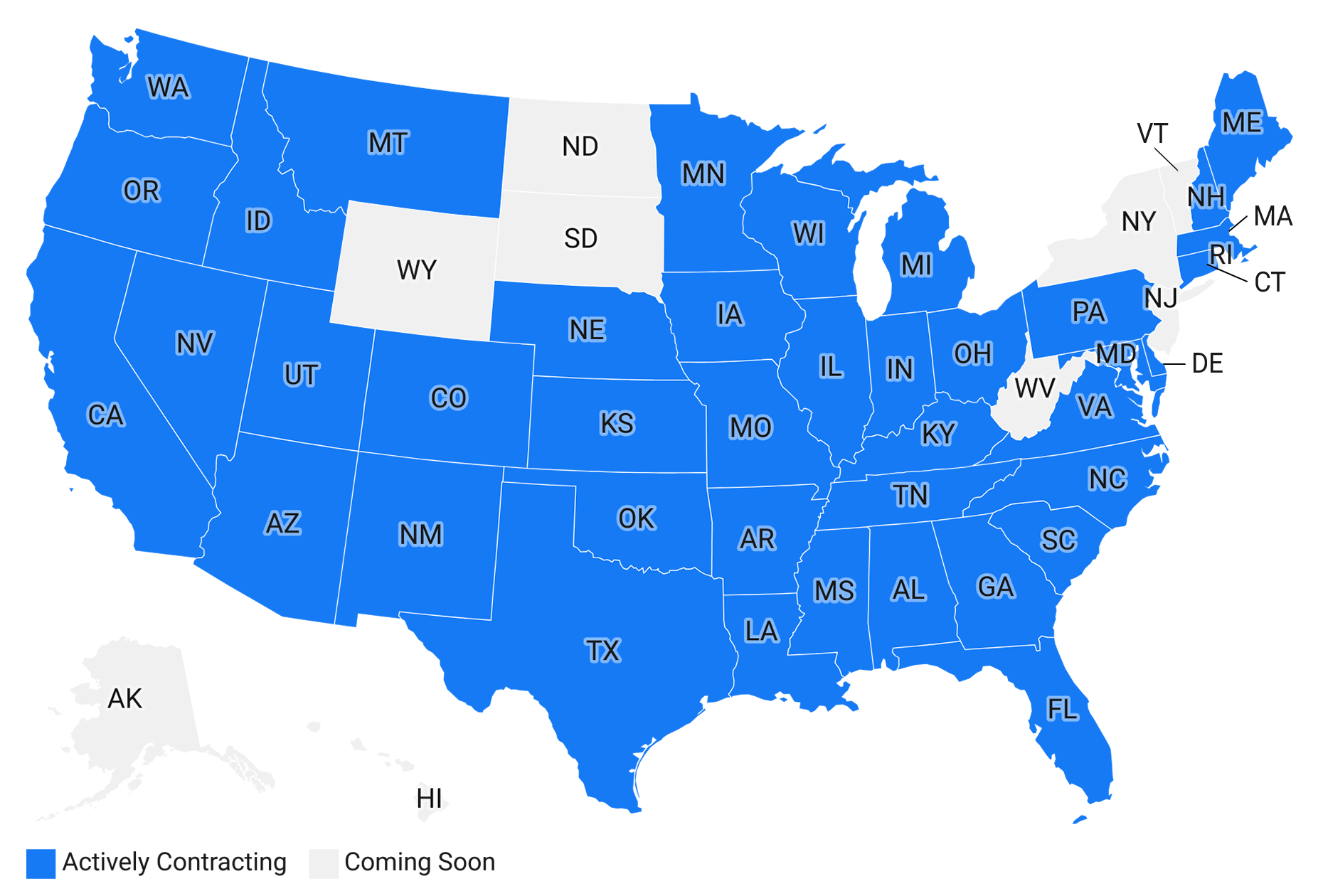
We’ve Got You Covered
Through our Network of independent DPC practices Hint Connect matches geographically diverse employers with doctors across the country through a single contract that standardizes the benefit across all of the independent clinicians.
See where our clinicians are located today with our Network map.

Support the entire patient care cycle
Engage With Patients Before & After Visits
Online scheduling, intake forms, lab results and prescription fills for your patients helps your practice stay connected to your panel.Virtual and In-Person Care
Provide a seamless care experience to both patients and clinicians, whether you're seeing patients virtually or in the clinic.Document Visits and Create Orders
Reduce clicks and documentation time with an intuitive and efficient system, purpose-built for primary care.See the Trends Driving Employer Adoption of DPC
DPC makes it easier for employees to access primary care on a regular basis, thereby increasing utilization, which results in less visits to expensive sites of care such as specialists, urgent care, emergency departments, and inpatient hospitals. Preventative care and any health issues can be addressed early on at the office of a DPC clinician, often at no additional charge.
The Hint Health Data Analytics team compiled data from over 6,000 employers, 3,500 DPC clinicians, and their 1,000,000+ members into the Employer Trends in Direct Primary Care 2023 to better understand changes, challenges, and benefits of employer-sponsored DPC.

Categories
Choose below
- All
- Captive
- Health Share
- TPA/Health Plan
- Benefits Advisor
- Innovator
Hint Connect Partners
Case Study
Learn how a DPC expanded its reach to support a 7-state employer using Hint Connect
View Case StudyWebinar
Watch the recording of Hint Connect's webinar with David Contorno of E Powered Benefits announcing the launch of E Powered DPC.
Watch NowPodcast
Beth Holmes, Head of Hint Connect, talks about how DPC is different, the benefits it brings to users, and how Hint Connect is positioned to bring the benefit of DPC to health plans.
Listen NowGet Started with Hint Connect
Submit your contact information, and a member of our team will be in touch to explore how you can help to make primary care more affordable and accessible to all.
If you're a clinician interested in joining Hint Connect, visit our Hint Connect for clinicians page.




.png)








